IMPORTANT UPDATE FOR SCHOOLS CDC recommends schools continue to use the current COVID-19 prevention strategies for the 2021 school year

Operational Strategy for K-12 Schools through Phased Prevention
Summary of Recent Changes
CDC recommends schools continue to use the current COVID-19 prevention strategies for the 2020-2021 school year.
Key Points
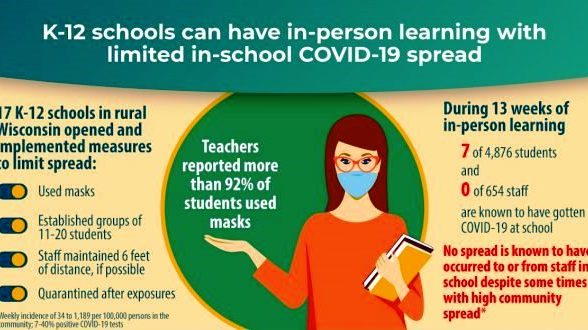
- Evidence suggests that many K-12 schools that have strictly implemented prevention strategies have been able to safely open for in-person instruction and remain open.
- CDC’s K-12 operational strategy presents a pathway for schools to provide in-person instruction safely through consistent use of prevention strategies, including universal and correct use of masks and physical distancing.
- All schools should implement and layer prevention strategies and should prioritize universal and correct use of masks and physical distancing.
- Testing to identify individuals with SARS-CoV-2 infection and vaccination for teachers and staff provide additional layers of COVID-19 protection in schools.
- Essential Elements of Safe K–12 School Operations for In-Person Learning
- Health Equity Considerations
- Prevention Strategies to Reduce Transmission of SARS-CoV-2 in Schools
- Cleaning and maintaining healthy facilities
- Fully Vaccinated
- Indicators of Community Transmission
- Phased Prevention
- Additional COVID-19 Prevention Strategies in Schools
- Testing
- Vaccination for Teachers and School Staff
Essential Elements of Safe K–12 School Operations for In-Person Learning
Schools are an important part of the infrastructure of communities, as they provide safe and supportive learning environments for students, employ teachers and other staff, and enable parents, guardians, and caregivers to work. Many students, staff, and caregivers are either missing or have had interruptions in services due to school building closures and virtual and hybrid learning. Evidence suggests that many K–12 schools that have strictly implemented prevention strategies have been able to safely open for in-person instruction and remain open.1
CDC’s Science Brief on Transmission of SARS-CoV-2 in K–12 Schools summarizes evidence on COVID-19 among children and adolescents and what is known about preventing transmission in schools.
CDC has developed guidance for prevention strategies that K–12 school administrators can use to help protect students, teachers, and staff, and slow the spread of COVID-19. If prevention strategies are strictly adhered to, K–12 schools can safely open for in-person instruction and remain open.1 This document provides an operational strategy for safe delivery of in-person instruction in K–12 schools through the integration of a package of prevention and control components:
- Consistent implementation of layered prevention strategies to reduce SARS-CoV-2 transmission in schools
- Consideration of indicators of community transmission to reflect levels of community risk
- Phased prevention strategies based on levels of community transmission
The following public health efforts provide additional layers of COVID-19 protection in schools:
- Testing to identify individuals with a SARS-CoV-2 infection to limit transmission and outbreaks
- Vaccination for teachers and staff as soon as possible
Health Equity Considerations
Long-standing systemic health and social inequities have put many racial and ethnic minority groups at increased risk of getting sick and dying from COVID-19. People who identify as American Indian/Alaska Native, Black, and Hispanic are disproportionately affected by COVID-19; these disparities have also emerged among children.1 The absence of in-person educational options might disadvantage children from all backgrounds, particularly children in low-resourced communities who might be at an educational disadvantage. These students might be less likely to have access to technology to facilitate virtual learning and more likely to rely on key school-supported resources such as school meal programs, special education and related services, counseling, and after-school programs. Some parents and caregivers might have less-flexible jobs that do not permit staying at home to provide childcare and aid with virtual learning if schools are closed to in-person instruction. On the other hand, certain racial and ethnic groups have borne a disproportionate burden of illness and serious outcomes from COVID-19. These health disparities are evident even among school-aged children,1 suggesting that in-person instruction might pose a greater risk of COVID-19 to disproportionately affected populations. For these reasons, health equity considerations related to in-person instruction are an integral part of this complex decision-making. To enable in-person learning in schools that serve racial and ethnic groups disproportionately affected by COVID-19, school administrators and public health officials can work together to help schools plan and implement comprehensive prevention strategies, engage community partners, and assist with referrals to medical care. It is important that these schools have the resources and technical assistance needed to adopt and diligently implement actions to slow the spread of the virus that causes COVID-19 among people inside the school and out in the community. Schools play a critical role in promoting equity in education and health for groups disproportionately affected by COVID-19.
Engagement with educators, families, and the school community
A successful and equitable school reopening strategy requires engaging the entire school community to establish a safe environment for all educators, school staff, and students and promote trust and confidence. School reopening planning should include:
- Administrators
- Teachers
- Student and parent representatives
- Specialized instructional support personnel (such as school counselors, school social workers, school psychologists, and nurses)
- Facilities managers and custodial staff
- Transportation personnel, school nutrition professionals, and family services representatives.
Consistent with health equity considerations, schools and school districts should conduct active and specific outreach to underserved families – including parents/guardians of students of color, students from low-income backgrounds, students with disabilities, English learners, students experiencing homelessness, and students in foster care. This communication should be conducted in families’ home languages or mode of communication and in alternate formats as needed to facilitate effective communication for individuals with disabilities and, where appropriate, in partnership with trusted community-based organizations.
Prevention Strategies to Reduce Transmission of SARS-CoV-2 in Schools
Regardless of the level of community transmission, it is critical that schools use and layer prevention strategies. Five key prevention strategies are essential to safe delivery of in-person instruction and help to prevent COVID-19 transmission in schools:
- Universal and correct use of masks
- Physical distancing
- Handwashing and respiratory etiquette
- Cleaning and maintaining healthy facilities
- Contact tracing in combination with isolation and quarantine
Schools providing in-person instruction should prioritize two prevention strategies:
- Universal and correct use of masks should be required
- Physical distancing should be maximized to the greatest extent possible.
All prevention strategies provide some level of protection, and layered strategies implemented at the same time provide the greatest level of protection. Schools should adopt prevention strategies to the largest extent practical—a layered approach is essential.
Health equity considerations in prevention strategies
- Federal and state disability laws, to the extent applicable, require an individualized approach for students with disabilities consistent with the student’s IEP or Section 504 plan. Educators and school leaders must remain aware of their obligations under federal and state disability laws and should also consider adaptations and alternatives to prevention strategies, while maintaining efforts to protect students, teachers, and staff from COVID-19.
- CDC’s K–12 Schools COVID-19 Prevention Toolkitpdf icon includes resources, tools, and checklists to help school administrators and school officials prepare schools to open for in-person instruction and to manage ongoing operations. These tools and resources include considerations for addressing health equity, such as class sizes, internet connectivity, access to public transportation, etc.
Universal and correct use of masks
Core principle for masks: Require consistent and correct use of well-fitting face masks with proper filtration by all students, teachers, and staff to prevent SARS-CoV-2 transmission through respiratory droplets. Masks should be worn at all times, by all people in school facilities, with certain exceptions for certain people, or for certain settings or activities, such as while eating or drinking. Masks should be required in all classroom and non-classroom settings, including hallways, school offices, restrooms, gyms, auditoriums, etc.
- Mask policies for all students, teachers, and staff set the expectation that people will use masks throughout the school.
- The most effective fabrics for cloth masks are tightly woven, such as cotton and cotton blends, breathable, and in two or three fabric layers. Masks with exhalation valves or vents, those that use loosely woven fabrics, and those that do not fit properly are not recommended.
- Most students, including those with disabilities, can tolerate and safely wear a mask. However, a narrow subset of students with disabilities might not be able to wear a mask or cannot safely wear a mask. Those who cannot safely wear a mask—for example, a person with a disability who, for reasons related to the disability, would be physically unable to remove a mask without assistance if breathing becomes obstructed—should not be required to wear one. For the remaining portion of the subset, schools should make individualized determinations as required by Federal disability laws in order to determine if an exception to the mask requirement is necessary and appropriate for a particular student. If a child with a disability cannot wear a mask, maintain physical distance, or adhere to other public health requirements, the student is still entitled to an appropriate education, which in some circumstances may need to be provided virtually.
- Mask use should be required on school buses and other public transportation; school systems should take appropriate steps to ensure compliance with this requirement by students, staff, and others.
- If visitors are permitted in school, they should be required to wear masks at all times and should maintain physical distance from others.
- Schools should encourage modeling of correct and consistent mask use by school leaders, local leaders, and others respected in the community.


Find a mask that is made for children to help ensure proper fit. Check to be sure the mask fits snugly over the nose and mouth and under the chin and that there are no gaps around the sides.
Physical distancing
Core principle for physical distancing: Establish school policies and implement structural interventions to promote physical distance between people.
- Between students in classrooms
- In elementary schools, students should be at least 3 feet apart.1
- In middle schools and high schools, students should be at least 3 feet apart in areas of low, moderate, or substantial community transmission. In areas of high community transmission, middle and high school students should be 6 feet apart if cohorting is not possible.1,2, 4-6
- Maintain 6 feet of distance in the following settings:
- Between adults (teachers and staff), and between adults and students, at all times in the school building. Several studies have found that transmission between staff is more common than transmission between students and staff, and among students, in schools.1
- When masks cannot be worn, such as when eating.
- During activities when increased exhalation occurs, such as singing, shouting, band, or sports and exercise. Move these activities outdoors or to large, well-ventilated space, when possible.
- In common areas such as school lobbies and auditoriums.
- Use cohorting, and maintain 6 feet of distance between cohorts where possible. Limit contact between cohorts. In areas of substantial (orange) and high (red) levels of community transmission, schools that use less than 6 feet between students in classrooms, cohorting is recommended, with at least 6 feet maintained between cohorts.
- Remove nonessential furniture and make other changes to classroom layouts to maximize distance between students.
- Face desks in the same direction, where possible.
- Eliminate or decrease nonessential in-person interactions among teachers and staff during meetings, lunches, and other situations that could lead to adult-to-adult transmission.
- Visitors: Limit any nonessential visitors, volunteers, and activities involving external groups or organizations as much as possible—especially with people who are not from the local geographic area (for example, not from the same community, town, city, county). Require all visitors to wear masks and physically distance from others.
- Create distance between children on school buses when possible. Open windows to improve ventilation when it does not create a safety hazard.

Transportation: Create distance between children on school buses (for example, seat children one child per row, skip rows), when possible. Masks are required by federal order on school buses and other forms of public transportation in the United States. Open windows to improve ventilation when it does not create a safety hazard. More information about school transportation and prevention is available.
Additional suggestions for physical distancing:
- Staggered scheduling: Stagger school arrival and drop-off times or locations by cohort, or put in place other protocols to limit contact between cohorts, as well as direct contact with parents.
- Alternate schedules with fixed cohorts of students and staff to decrease class size and promote physical distancing.
Handwashing and respiratory etiquette
Core principle for handwashing and respiratory etiquette: Through ongoing health education units and lessons, teach children proper handwashing and reinforce behaviors, and provide adequate supplies. Ensure that teachers and staff use proper handwashing and respiratory etiquette.
- Teach and reinforce handwashing with soap and water for at least 20 seconds and increase monitoring to ensure adherence among students, teachers, and staff. If handwashing is not possible, hand sanitizer containing at least 60% alcohol should be used.
- Encourage students and staff to cover coughs and sneezes with a tissue when not wearing a mask and immediately wash their hands after blowing their nose, coughing, or sneezing.
- Some students with disabilities might need assistance with handwashing and respiratory etiquette behaviors.
- Adequate supplies: Support healthy hygiene behaviors by providing adequate supplies, including soap, a way to dry hands, tissues, face masks (as feasible), and no-touch/foot-pedal trash cans. If soap and water are not readily available, schools can provide alcohol-based hand sanitizer that contains at least 60% alcohol (for staff and older children who can safely use hand sanitizer).
Cleaning and maintaining healthy facilities
Core principle for cleaning and maintaining healthy facilities: Make changes to physical spaces to maintain a healthy environment and facilities, including improving ventilation. Routinely clean high-touch surfaces (such as doorknobs and light switches).
- Ventilation: Improve ventilation to the extent possible to increase circulation of outdoor air, increase the delivery of clean air, and dilute potential contaminants. This can be achieved through several actions.
- Bring in as much outdoor air as possible.
- Ensure Heating, Ventilation, and Air Conditioning (HVAC) settings are maximizing ventilation.
- Filter and/or clean the air in the school by improving the level of filtration as much as possible.
- Use exhaust fans in restrooms and kitchens.
- Open windows in buses and other transportation, if doing so does not pose a safety risk. Even just cracking windows open a few inches improves air circulation.
- Modified layouts: Adjust physical layouts in classrooms and other settings to maximize physical space, such as by turning desks to face in the same direction.
- Cleaning: Regularly clean high touch surfaces and objects (for example, playground equipment, door handles, sink handles, toilets, drinking fountains) within the school and on school buses at least daily or between use as much as possible.
- Communal spaces: Close communal use of shared spaces, such as cafeterias, if possible; otherwise, stagger use and clean regularly (for example, daily or as often as needed). Consider use of larger spaces such as cafeterias, libraries, gyms for academic instruction, to maximize physical distancing.
- Food service: Avoid offering any self-serve food or drink options such as hot and cold food bars, salad or condiment bars, and drink stations.
- Water systems: Take steps to ensure that all water systems and features (for example, sink faucets, decorative fountains) are safe to use after a prolonged facility shutdown.


Before students and staff return to a school or childcare building that has been closed for an extended time, look for ways to reduce potential hazards. Flush plumbing (including all sink faucets, water fountains, water bottle fillers, hoses, and showers) to replace all water inside building pipes with fresh water. This can help protect occupants from possible exposure to lead, copper, and Legionella bacteria. You can also follow the U.S. Environmental Protection Agency (EPA) 3Ts – Training, Testing, and Taking Actionexternal icon – for reducing lead in drinking water at schools and childcare centers. Follow guidance to check your building for mold and remediate as needed.
Contact tracing in combination with isolation and quarantine
Core principle for contact tracing: Schools should collaborate with the health department, to the extent allowable by privacy laws and other applicable laws, to confidentially provide information about people diagnosed with or exposed to COVID-19. Students, teachers, and staff with positive test results should isolate, and close contacts should quarantine. Schools should report positive cases to the health department as soon as they are informed. School officials should notify families of close contacts as soon as possible after they are notified that someone in the school has tested positive (within the same school day).
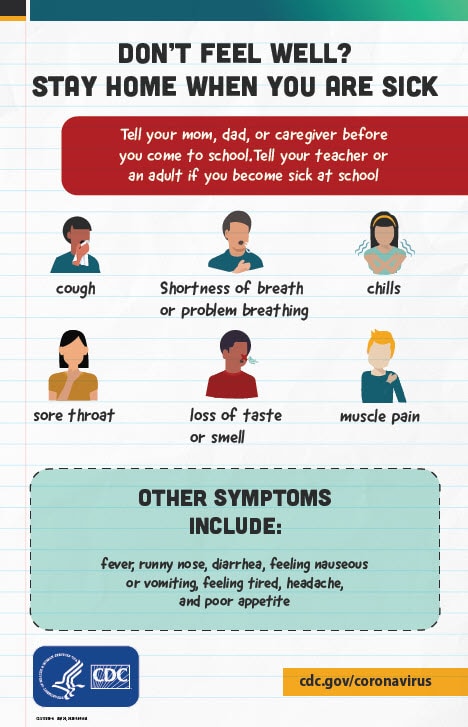
Don’t Feel Well? Poster encourages students to tell a teacher if they feel sick
- Staying home when appropriate: Educate teachers, staff and families about when they and their children should stay home and when they can return to school. Students, teachers, and staff who have symptoms should stay home and be referred to their healthcare provider for testing and care. Schools may need to consider flexible sick leave policies and practices that enable teachers and staff to stay home when they are sick, have been exposed, or are caring for someone who is sick. School systems should recruit and train sufficient substitute educators to ensure that teachers can stay home when they are sick or have been exposed to someone who is confirmed or suspected of having COVID-19.
- Isolation should be used to separate people diagnosed with COVID-19 from those who are not infected. Students, teachers, and staff who are in isolation should stay home and follow the direction of the local public health authority about when it is safe for them to be around others.
- Case investigation and contact tracing: Schools should work with the local health department to facilitate, to the extent allowable by applicable laws, systematic case investigation and contact tracing of infected students, teachers, and staff, and consistent isolation of cases and quarantine of close contacts. Schools can prepare and provide information and records to aid in the identification of potential contacts and exposure sites, consistent with applicable laws, including those related to privacy and confidentiality. Collaboration between the health department and K-12 school administration to obtain contact information of other individuals in shared rooms, class schedules, shared meals, or extracurricular activities will expedite contact tracing. For schools to remain open, health departments should ensure they have enough contact tracers to complete case investigation and notify contacts within 48 hours of a positive test result. Prompt identification, quarantine, and monitoring of those contacts exposed to SARS-CoV-2 can effectively break the chain of transmission and prevent further spread of the virus
- The definition of a close contact is someone who was within 6 feet of a person diagnosed with COVID-19 for a total of 15 minutes or more over a 24 hour period. The definition of a close contact applies regardless of whether either person was wearing a mask.
- For schools that use less than 6 feet between students in classrooms, the definition of close contacts should not change. Students sitting less than 6 feet next to another student or person diagnosed with COVID-19 for a total of 15 minutes or more should quarantine at home and be referred for testing.
- Quarantine should be used for students, teachers, and staff who might have been exposed to COVID-19. Close contacts, identified through contact tracing, should quarantine unless they are fully vaccinated, or have tested positive in the last 3 months, and do not have any symptoms. Students, teachers, and staff who are in quarantine should stay home and follow the direction of the local public health department about when it is safe for them to be around others. If a child with a disability is required to quarantine, the school is required to provide services consistent with federal disability laws.
Fully Vaccinated
CDC recently released guidance on the ability of fully vaccinated people to resume pre-pandemic activities without wearing a mask or physically distancing, except where required by federal, state, local, tribal, or territorial laws, rules, and regulations, including local business and work place guidance. This guidance has raised questions for schools about how to proceed in the current school year. CDC recommends schools continue to use the COVID-19 prevention strategies outlined in the current version of CDC’s Operational Strategy for K-12 Schools for at least the remainder of the 2020-2021 academic school year.
Recommendation for continuation with these prevention strategies is based on
- Students will not be fully vaccinated by the end of the 2020-2021 school year. Youth under the age of 12 are not yet eligible for vaccination. Youth between the ages of 12 and 15 became eligible for vaccination on May 12, 2021. Because people are not fully vaccinated until 2 weeks after their second dose of the Pfizer vaccine, students in this age group will not be fully vaccinated before the end of current school year.
- The time needed for schools to make systems and policy adjustments. Systems and policy adjustments may be required for schools to change mask requirements for students and staff while continuing to ensure the safety of unvaccinated populations.
CDC will update its guidance for schools in the coming weeks. Updated guidance can inform school planning for the 2021-2022 academic year.
Indicators of Community Transmission
School administrators, working with local public health officials, should assess the level of community transmission to understand the burden of disease in the community. The higher the level of community transmission, the more likely that SARS-CoV-2 will be introduced into the school facility from the community, which could lead to in-school transmission if layered prevention strategies are not in use.
CDC recommends the use of two measures of community burden to determine the level of risk of transmission: total number of new cases per 100,000 persons in the past 7 days, and percentage of nucleic acid amplification tests (NAATs), including RT-PCR tests, that are positive during the last 7 days. The two measures of community burden should be used to assess the incidence and spread of SARS-CoV-2 in the surrounding community (for example, county) and not in the schools themselves. If the two indicators suggest different levels, the actions corresponding to the higher threshold (in Table 2) should be chosen. The transmission level for any given location will change over time and should be reassessed weekly for situational awareness and to continuously inform planning and decision-making.
Table 1. CDC Indicators and Thresholds for Community Transmission of COVID-191
| Indicator | Low TransmissionBlue | Moderate TransmissionYellow | Substantial TransmissionOrange | High TransmissionRed |
|---|---|---|---|---|
| Total new cases per 100,000 persons in the past 7 days2 | 0-9 | 10-49 | 50-99 | ≥100 |
| Percentage of NAATs that are positive during the past 7 days3 | <5.0% | 5.0%-7.9% | 8.0%-9.9% | ≥10.0% |
1If the two indicators suggest different levels, the actions corresponding to the higher threshold should be chosen. County-level data on total new cases in the past 7 days and test percent positivity are available on the County View tab in CDC’s COVID Data Tracker.
2Total number of new cases per 100,000 persons within the last 7 days is calculated by adding the number of new cases in the county (or other community type) in the last 7 days divided by the population in the county (or other community type) and multiplying by 100,000.
3Percentage of positive diagnostic and screening NAATs during the last 7 days is calculated by dividing the number of positive tests in the county (or other administrative level) during the last 7 days by the total number of tests resulted over the last 7 days. Additional information can be found on the Calculating Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Laboratory Test Percent Positivity: CDC Methods and Considerations for Comparisons and Interpretation webpage.
Phased Prevention
A phased prevention approach for K–12 schools relies on several core concepts.
- K–12 schools should be the last settings to close after all other prevention measures in the community have been employed, and the first to reopen when they can do so safely. This implies that decision-makers and communities should prioritize schools for reopening and remaining open for in-person instruction over nonessential businesses and activities, including indoor dining, bars, social gatherings, and close contact sports as community transmission is controlled.
- In-person instruction should be prioritized over extracurricular activities, including sports and school events, to minimize risk of transmission in schools and protect in-person learning. Prolonged periods of remote or virtual learning can have negative effects on educational progress for students, potentially slowing or reversing academic gains. Students from low-resourced communities, English learners, and students with disabilities might disproportionately experience learning loss due to limited access to remote learning technology and fewer learning support systems and services outside of schools. Safe in-person schooling can also offset the negative social, emotional, and mental health impacts of prolonged virtual learning. Minimizing the risk of spread during extracurricular activities and social gatherings outside of school can help maintain in-person instruction. Some close-contact sports might not be able to be implemented at any level of community transmission given the risk of transmission and the inability to implement prevention strategies.1 Schools may consider using expanded screening testing for sports and extracurricular activities to identify cases and reduce risk of transmission from people who are asymptomatic or pre-symptomatic.
- Lower susceptibility and incidence among younger children compared to teenagers suggests that younger students (for example, elementary school students) are likely to have less risk of in-school transmission due to in-person learning than older students (middle schools and high schools). In addition, younger children may benefit more from in-person instruction and are less independent than older students.
- Families of students who are at increased risk of severe illness (including those with special healthcare needs) or who live with people at high risk should be given the option of virtual instruction, regardless of the mode of learning offered.
- Schools are encouraged to use cohorting, especially in areas of substantial (orange) and high (red) transmission, to facilitate testing and contact tracing, and to minimize transmission across cohorts.
Monitoring levels of community transmission provides school leaders with an indicator system for the risk of introduction of SARS-CoV-2 virus into a school. Information about levels of community transmission should be combined with information about cases in schools and implementation of prevention strategies to guide decision-making. Implementation of prevention strategies should be intensified if indicators worsen (i.e., moving from low to moderate to substantial to high community transmission). Intensifying prevention might also involve imposing restrictions on sports and extracurricular activities to protect in-person learning. To make decisions about preventive actions, school and health officials should take the following information into account:
- The numbers of COVID-19 cases among students, teachers, and staff, and number of people in quarantine
- Compliance with prevention strategies
- Levels of community transmission
Table 2 presents a school operational plan for opening and remaining open that emphasizes layering prevention at all levels of community transmission.
Table 2. Recommended Prevention Strategies for K-12 Schools and Levels of Community Transmission
| Prevention Strategies: All Schools | |||
All schools implement 5 key prevention strategies:
|
|||
| Prevention Strategies by Level of Community Transmission | |||
| Low Transmission1Blue | Moderate TransmissionYellow | Substantial TransmissionOrange | High TransmissionRed |
|---|---|---|---|
| Elementary SchoolsPhysical distancing: at least 3 feet between students in classrooms | Elementary SchoolsPhysical distancing: at least 3 feet of distance between students in classrooms
Cohorting2 recommended when possible |
||
| Middle and High SchoolsPhysical distancing: at least 3 feet between students in classrooms | Middle and High SchoolsPhysical distancing: at least 3 feet of distance between students in classrooms
Cohorting recommended when possible |
Middle and High SchoolsSchools that can use cohorting: at least 3 feet of distance
Schools that cannot use cohorting: at least 6 feet distance between students in classrooms 2 |
|
| Sports and extracurricular activitiesSports and extracurricular activities occur with at least 6 feet of physical distance to the greatest extent possible6 | Sports and extracurricular activitiesSports and extracurricular activities occur with at least 6 feet of physical distance required6 | Sports and extracurricular activitiesSports and extracurricular activities occur only if they can be held outdoors, with more than 6 feet of physical distancing6 | |
1Levels of community transmission defined as total new cases per 100,000 persons in the past 7 days (low, 0-9; moderate, 10-49; substantial, 50-99; high, ≥100) and percentage of positive tests in the past 7 days (low, <5%; moderate, 5-7.9%; substantial, 8-9.9%; high, ≥10%).
2Cohorting involves creating groups of students that are separated from other groups by at least 6 feet throughout the entire day. Cohorting can be implemented in either full in-person instruction or hybrid instruction, or through other strategies.
3In middle and high schools, 6 feet is recommended in areas of high community transmission, unless they can implement cohorting. Schools may consider using reduced attendance, hybrid instruction, or other strategies to ensure 6 feet of physical distance between students in middle and high schools that do not use cohorting. Diagnostic testing for SARS-CoV-2 is intended to identify occurrence of SARS-CoV-2 infection at the individual level and is performed on individuals with or without suspected COVID-19 infection in accordance with the test’s authorization and labeling.
4Middle and high schools in areas of high community transmission should implement cohorting if they use less than 6 feet between students in classrooms. If cohorting is not possible, 6 feet between students is recommended. Middle and high schools can use strategies such as reduced attendance (some students are virtual only at all times) or hybrid instruction to achieve 6 feet of distance.
5School officials should implement limits on spectators and attendees for sports, extracurricular activities, and events to ensure 6 feet of physical distance and require use of masks.
6Schools may consider using screening testing for student athletes and adults (e.g., coaches, trainers) who support these activities to facilitate safe participation and reduce risk of transmission. See screening testing section and Table 4 for additional details.
Monitoring cases and making decisions about in-person instruction
Schools should closely and regularly monitor the numbers of students, teachers, and staff with COVID-19, as well those in isolation and in quarantine. In collaboration with the local health department, decisions should combine information about levels of community transmission with school-specific factors, such as implementation of prevention strategies and the number of cases among students, teachers, and staff. Schools may consider convening a team or committee with representation from local public health and members of the school community (for example, students, parents, teachers, and staff) to review data regularly, share information, and discuss opportunities to support open communication with school stakeholders. As levels of community transmission increase, schools should further strengthen prevention strategies and monitor cases to reassess decisions.
Interventions to control clusters
A school cluster is an index case and two or more cases epidemiologically linked to the index case who likely acquired SARS-CoV-2 infection in school (i.e., school-associated cases). When cases are introduced into the school environment, they can lead to clusters and potentially to rapid and uncontrolled spread. This is more likely to happen in areas of substantial or high community transmission, as cases are more likely to be introduced into the school from the community. Schools should monitor cases (consistent with privacy and other applicable laws), identify clusters quickly, and promptly intervene to control spread. Infection source and whether the infection is likely acquired in school or outside of school should be determined by case investigations conducted by a collaboration between school administration and the local health department.
Schools should take the following actions to control transmission in the event of a cluster:
- Investigate cases and trace contacts; encourage isolation and quarantine (consistent with applicable privacy and other laws).
- Work with the health department to carefully investigate each case, including conducting interviews with students, teachers, parents, and school staff.
- Encourage compliance with isolation for people who test positive.
- Work with the health department to trace close contacts in accordance with applicable federal and state privacy laws of all cases and refer close contacts for diagnostic testing. Encourage compliance with quarantine.
- Assess situations where close contacts occurred and implement interventions to address potential contributors to the clusters. For example:
- Determine whether inconsistent or incorrect use of masks contributed to the clusters and intervene to improve consistent and correct mask use.
- Assess implementation of physical distancing and determine whether intervention is needed to address distancing.
- Eliminate or decrease nonessential in-person interactions among teachers and staff during meetings, lunches, and other situations that may have led to adult-to-adult transmission.
Unplanned school closures

In cases where schools must temporarily close for in-person instruction, schools should make efforts to provide continuity of instruction through synchronous remote learning or at-home activities.
Despite careful planning and consistent implementation of prevention strategies, some situations may lead school officials to consider temporarily closing schools or parts of a school (such as a class, cohort, or grade level) to in-person instruction, typically in consultation with the local health department. These decisions should be made based on careful consideration of a variety of factors and with the emphasis on ensuring the health and wellness of students, their families, and teachers and staff. In such cases, schools should make efforts to provide continuity of instruction through synchronous remote learning or at-home activities.
Classrooms, cohorts, or schools experiencing uncontrolled spread of COVID-19 may temporarily close for in-person learning. If the school is experiencing uncontrolled spread, school leaders should immediately notify public health officials and collaborate to facilitate increased testing and contact tracing, as necessary. The local health department may facilitate testing for students, teachers, and staff who are in schools with an uncontrolled spread.
Schools in areas experiencing rapid or persistent rises in COVID-19 case rates or severe burden on health care capacity. School leaders and public health officials should monitor indicators of community transmission (Table 1) and review trends over time. In communities that have rapid or persistent rises in COVID-19 incidence or severe healthcare capacity burden, school leaders may decide to temporarily close schools to in-person instruction until levels of community transmission stabilize.
Providing options for teachers and school staff
At all levels of community transmission, employers should provide reassignment, remote work, or other options for teachers and staff who have documented high-risk conditions that place them at increased risk for severe illness from COVID-19 to limit the risk of workplace exposure. When these conditions are disabilities under the Americans with Disabilities Act, employers should ensure compliance with law and may need to consider providing reasonable accommodation subject to undue hardship. Options for reassignment may include but are not limited to telework, virtual teaching opportunities, modified job responsibilities, environmental modifications, scheduling flexibility, or temporary reassignment to different job responsibilities. These options should likewise be extended to teachers and staff who have a household member who is at increased risk for severe illness from COVID-19. Policies and procedures addressing issues related to teachers and staff at higher risk of serious illness and the application of reassignment, remote work, or other options for prevention should be made in consultation with occupational medicine and human resource professionals with knowledge of the specific situation, keeping in mind Equal Employment Opportunity (EEO) and other potential legal concerns. Schools should work with local counsel to ensure compliance.
New COVID-19 variants and prevention in schools
Multiple SARS-CoV-2 variants are circulating globally. These include several variants that have been detected in the United States. Some of these variants seem to spread more easily and quickly than other variants, which could lead to more cases of COVID-19. Rigorous implementation of prevention strategies is essential to control the spread of variants of SARS-CoV-2. CDC, in collaboration with other public health agencies, is monitoring the situation closely and studying these variants quickly to learn more to control their spread. As more information becomes available, prevention strategies and school guidance may need to be adjusted to new evidence on risk of transmission and effectiveness of prevention in variants that are circulating in the community.
Health equity considerations in phased prevention
- Schools that serve student populations that are at greater risk for learning loss during virtual instruction (for example, due to their more limited access to technology) should be prioritized for providing in-person instruction and be provided the needed resources to implement prevention.
- Schools should consider prioritizing in-person instruction for students with disabilities who require special education and related services directly provided in school environments, as well as other students who may benefit from receiving essential instruction in a school setting.
- Schools should develop plans to continue meal service provision, such as free breakfast and lunch to families for every learning mode, including in-person, hybrid, and virtual.
Additional COVID-19 Prevention Strategies in Schools
Testing
Viral testing strategies in partnership with schools should be part of a comprehensive prevention approach. Testing should not be used alone, but in combination with other prevention to reduce risk of transmission in schools. When schools implement testing combined with prevention strategies, they can detect new cases to prevent outbreaks, reduce the risk of further transmission, and protect students, teachers, and staff from COVID-19.
Diagnostic Testing
At all levels of community transmission, schools should offer referrals to diagnostic testing to any student, teacher, or staff member who is exhibiting symptoms of COVID-19 at school. Diagnostic testing for SARS-CoV-2 is intended to identify occurrence of SARS-CoV-2 infection at the individual level and is performed when there is a reason to suspect that an individual may be infected, such as having symptoms or suspected recent exposure. Examples of diagnostic testing strategies include testing symptomatic teachers, students, and staff who develop symptoms in school, and testing asymptomatic individuals who were exposed to someone with a confirmed or suspected case of COVID-19. Additional considerations for diagnostic testing:
- Schools should advise students, teachers, and staff to stay home if they are sick or if they have been exposed to SARS-CoV-2. Schools can encourage these individuals to talk to their healthcare provider about getting a COVID-19 test.
- If a student, teacher, or staff member becomes sick at school or reports a new COVID-19 diagnosis, schools should follow the steps of the COVID-19 Diagnosis flowchart on what to do next. This includes notifying a student’s parent or guardian and initiating testing strategies. Notifications must be accessible for all students, parents, or guardians, including those with disabilities or limited English proficiency (for example, through use of interpreters or translated materials).
- In some schools, school-based healthcare professionals (for example, school nurses) may perform SARS-CoV-2 antigen testing in school-based health centers if they are trained in specimen collection, conducting the test per manufacturer’s instructions, and obtain a Clinical Laboratory Improvement Amendments (CLIA) certificate of waiverexternal icon. Some school-based healthcare professionals may also be able to perform specimen collection to send to a lab for testing, if trained in specimen collection, without a CLIA certificate. It is important that school-based healthcare professionals have access to, and training on the proper use of personal protective equipment (PPE).
- Not every school or school-based healthcare professional will have the staff, resources, or training to conduct testing. Public health officials should work with schools to help link students and their families, teachers, and staff to other opportunities for testing in their community. Testing could be offered by referral to community-based testing sites, through collaboration with local public health, or through a centralized test location offered by the school district.
The presence of any of the symptoms below generally suggests a student, teacher, or staff member has an infectious illness and should not attend school, regardless of whether the illness is COVID-19. For students, staff, and teachers with chronic conditions, symptom presence should represent a change from their typical health status to warrant exclusion from school. Occurrence of any of the symptoms below while a student, teacher, or staff member is at school suggests the person may be referred for diagnostic testing.
- Temperatureexternal iconof 100.4 degrees Fahrenheit or higher
- Sore throat
- Cough (for students with chronic cough due to allergies or asthma, a change in their cough from baseline)
- Difficulty breathing (for students with asthma, a change from their baseline breathing)
- Diarrhea or vomiting
- New loss of taste or smell
- New onset of severe headache, especially with a fever
Students should not attend school in-person if they or their caregiver identifies new development of any of the symptoms above.
Schools can provide options to separate students with COVID-19 symptoms or suspected or confirmed COVID-19 diagnoses by, for example, placing students in isolation room/areas until transportation can be arranged to send them home or seek emergency medical attention.
If a COVID-19 diagnosis is confirmed, schools can support public health officials in determining which close contacts and other potentially exposed persons in the school setting could be tested and either isolated or quarantined (see Table 3). Schools can assist by providing information, where appropriate, to identify close contacts (for example, class rosters, seating charts, and information to facilitate outreach to contacts).
Table 3. Tiered approach of diagnostic testing for SARS-CoV-21,2
| Students, teachers, and staff with symptoms of COVID-19 Refer for diagnostic testing |
Students, teachers, or staff with symptoms of COVID-19 at school, at all levels of community transmission.
|
| Close contacts Refer for diagnostic testing |
Students, teachers, or staff who had contact with someone diagnosed with COVID-19, defined as someone who has been within 6 feet of an infected person for a cumulative total of 15 minutes or more over a 24-hour period. The definition of a close contact applies regardless of whether either person was wearing a mask. The definition also applies in schools that use less than 6 feet between students in classrooms. Families of close contacts should be notified and referred for testing immediately.
|
1The tiers above are intended to be applied across all levels of community transmission: low (blue), moderate (yellow), substantial (orange), and high (red).
2 information should be provided with appropriate safeguards to protect personally identifiable information and HIPPA-sensitive information from unlawful release.
For diagnostic testing, selection of tests should prioritize tests with highly accurate results with high sensitivity and specificity such as NAATs. Referral to diagnostic testing for students, teachers, and staff who have symptoms of COVID-19 at school and for close contacts is recommended for all levels of community transmission. Students, teachers, and staff who have diagnostic testing performed should be isolated away from others and quarantined at home until test results are received. Diagnostic testing turnaround times depend on the type of test and the laboratory conducting it. Local capacity in diagnostic tests should ensure that people with suspected COVID-19 and their contacts are tested with results returning within 48 hours. At low levels of community transmission (blue), schools should refer students, teachers, and staff with symptoms or recent history of close contact with a confirmed case for diagnostic testing to identify or rule out SARS-CoV-2 infection. At moderate (yellow), substantial (orange), and high (red) levels, and at low (blue) levels for teachers and staff, referral to diagnostic testing is combined with screening testing to monitor any increases in infection rates.
For students, teachers, and staff who had previously received positive test results and do not have symptoms of COVID-19, retesting is not recommended for up to 3 months from their last positive test result. Data currently suggest that some individuals persistently test positive due to residual virus material but are unlikely to be infectious. Parents or guardians can request documentation from their healthcare provider to indicate the date and type of the student’s most recent COVID-19 test. Guidance on testing strategies for people who are fully vaccinated will be updated as more information becomes available. As vaccine supply increases and more teachers and staff receive vaccine, CDC’s priorities for SARS-CoV-2 testing will change and the guidance will be updated.
Screening Testing
Some schools may also elect to use screening testing as a strategy to identify cases and prevent secondary transmission. Screening testing involves using SARS-CoV-2 viral tests (diagnostic tests used for screening purposes) intended to identify occurrence at the individual level even if there is no reason to suspect infection—i.e., there is no known exposure and no symptoms. This includes, but is not limited to, screening testing of asymptomatic people without known exposure with the intent of making decisions based on the test results. Screening testing is intended to identify infected people without symptoms (or before development of symptoms) who may be contagious so that measures can be taken to prevent further transmission. The intent is to use the screening testing results to determine who may return to in-person school or work and the protective measures that will be taken, and to identify and isolate positive persons to prevent spread.
Screening testing is particularly valuable in areas with moderate, substantial, and high levels of community transmission. Screening testing for K–12 schools may allow schools to move between different testing strategies as community prevalence (and therefore risk assessment) changes. Screening testing could provide added protection for schools that use less than 6 feet of physical distancing between students in classrooms. For schools that implement it, screening testing should be offered at moderate (yellow), substantial (orange), and high (red) levels of community transmission, to students, teachers, and staff, and at low (blue) levels to teachers and staff. Achieving substantial reduction in transmission with testing requires more frequent testing and shorter lags between test administration and reporting of results.
Schools may consider using pooled testing as a screening testing strategy for students. Pooled testing involves mixing several samples from different individuals together in a “batch” or pooled sample, then testing the pooled sample with a diagnostic test. This approach increases the number of individuals that can be tested and reduces the need for testing resources. This approach may be particularly helpful in schools using cohorts. Because of the complexities of acting on a positive result, pooled testing is best used in situations where the number of positives is expected to be very low. Cohorts could be established in grade groups, such as all students in a particular grade or in similar grades (for example, K–grade 2; grades 3–5). If a confirmed positive case is found, close contacts of anyone in that cohort should be quarantined and tested.
Table 4. Testing Recommendations by Level of Community Transmission
| Testing Recommendations: All Schools | |||
| Diagnostic testing1: Symptomatic students, teachers, and staff and close contacts referred for diagnostic testingScreening Testing for teachers and staff: expanded screening testing3 of teachers and staff offered at least once per week | |||
| Testing Recommendations by Level of Community Transmission | |||
| Low Transmission1Blue | Moderate TransmissionYellow | Substantial TransmissionOrange | High TransmissionRed |
|---|---|---|---|
| No screening testing for students | Screening testing for students: expanded screening testing of students 4 offered at least once per week | ||
| Testing for high-risk sports:5 for schools conducting routine testing for sports, testing is recommended at least once per weekTesting for low and intermediate-risk sports: for schools conducting routine testing for sports, testing is recommended at least once per week | Testing for high-risk sports: for schools conducting routine testing for sports, testing is recommended twice per weekTesting for low and intermediate-risk sports: for schools conducting routine testing for sports, testing is recommended at least once per week | ||
1Diagnostic testing for SARS-CoV-2 is intended to identify occurrence of SARS-CoV-2 infection at the individual level and is performed when there is a reason to suspect that an individual may be infected, such as having symptoms or suspected recent exposure.
1Screening testing is intended to identify infected asymptomatic individuals who may be contagious so that measures can be taken to prevent further transmission.
3Levels of community transmission defined as total new cases per 100,000 persons in the past 7 days (low, 0-9; moderate, 10-49; substantial, 50-99; high, ≥100) and percentage of positive tests in the past 7 days (low, <5%; moderate, 5-7.9%; substantial, 8-9.9%; high, ≥10%).
4Schools may consider testing a random sample of at least 10% of students or may conduct pooled testing of cohorts/pods for screening testing in areas of moderate and substantial community transmission.
5Schools may consider using screening testing for student athletes and adults (e.g., coaches, teacher advisors) who support these activities to facilitate safe participation and reduce risk of transmission. For an example risk stratification for sports, see https://ncaaorg.s3.amazonaws.com/ssi/COVID/SSI_ResocializationDevelopingStandardsSecondEdition.pdfpdf iconexternal icon.
When combined with prevention measures, such as mask use, physical distancing, and others, testing protocols might be an effective tool in reducing transmission. Screening testing can be administered directly at a school facility (see Feasibility considerations section below), at a central location through the school district, or through referral to community-based testing providers.
- Moderate (yellow), substantial (orange), and high (red) community transmission: Students, teachers, and staff participate in regular screening testing to reduce the risk of transmission within the school.
- Teachers and staff participate in routine screening testing at least once per week. In areas with substantial and high community transmission, twice a week screening testing might be preferable to quickly detect cases among teachers and staff.
- Students in elementary, middle, and high schools participate in routine screening testing at least once per week. If a confirmed positive case is found, any close contacts are quarantined and tested.
- Schools might consider testing a random sample of at least 10% of students. For example, a school might randomly select 20% of the students each week for testing out of the entire population of students attending in-person instruction. Alternatively, a school might select one cohort for each grade level each week for testing. Different strategies for random selection can be used based on most adequate fit for a school screening testing strategy.
- Screening testing for sports: To facilitate safe participation in sports and reduce transmission in activities that have elevated risk, schools may consider requiring screening testing for participation. Schools can implement testing among student athletes/participants, coaches, and trainers, and any other individuals (such as parent volunteers) who could come into close contact with others during these activities.
- Sports events, competitions, and activities could include universal screening testing the day of the event or one day before.
- Low and intermediate risk sports3 include those that can be conducted outdoors, or indoors with masks. Testing at least once per week is recommended for these sports.
- High-risk sports3 include those that cannot be done outdoors or with masks. Testing twice per week in areas of low, moderate, and substantial community transmission is recommended for participation in these sports. High-risk sports should be virtual or canceled in areas of high community transmission.
When considering which tests to use for screening testing, schools or their testing partners should choose tests that can be reliably supplied and that provide results within 24 hours. NAATs are high-sensitivity tests for detecting SARS-CoV-2 nucleic acid. Most NAATs need to be processed in a laboratory with variable time to results (could be 1–3 days), but some NAATs are point-of-care tests with results available in about 15 minutes. Pooled testing—in which samples from multiple people are initially combined—may reduce costs and turn-around times. These may be considered for at least weekly screening testing in areas of moderate (yellow) community transmission.
Antigen tests are generally less sensitive than NAATs, and most can be processed at the point-of-care with results available in about 15 minutes. Antigen test results might need confirmation with a NAAT in certain circumstances, such as a negative test in persons with symptoms or a positive test in persons without symptoms. Schools should work with the health department to develop a confirmation and referral plan before implementing testing. The immediacy of results (test results in 15–30 minutes), modest costs, and feasibility of implementation of antigen tests make them a reasonable option for school-based screening testing. The feasibility and acceptability of tests that use nasal (anterior nares) swabs make these types of tests more readily implemented in school settings. Tests that use saliva specimens might also be acceptable alternatives for younger children, if tests are available and results are returned within 24 hours.
Taking into consideration the potential for limited availability of supplies for screening testing or feasibility of implementing screening testing, schools should consider a prioritization strategy.
- Schools and public health officials might consider prioritizing teachers and staff over students given the increased risk of severe illness among certain adults.
- In selecting among students, schools and public health officials might prioritize high school students, then middle school students, and then elementary school students, reflecting higher infection rates among adolescents compared to younger children.
Reporting test results
Every COVID-19 testing site is required to report to the appropriate state or local health officials all diagnostic and screening tests performed. Schools that use antigen testing must apply for and receive a Clinical Laboratory Improvement Amendments (CLIA)external icon certificate of waiver, and report test results to state or local public health departments as mandated by the Coronavirus Aid, Relief, and Economic Security (CARES) Act (P.L. 116-136).
Parents should be asked to report positive cases to schools to facilitate contact tracing and ensure communication and planning in schools. In addition, school administrators should notify staff, teachers, families, and emergency contacts or legal guardians immediately of any case of COVID-19 while maintaining confidentiality in accordance with the Health Insurance Portability and Accountability Act of 1996 (HIPAAexternal icon), the Americans with Disabilities Act (ADAexternal icon), and the Family Educational Rights and Privacy Act (FERPApdf iconexternal icon), and other applicable laws and regulations. Notifications must be accessible for all students, teachers, and staff, including those with disabilities or limited English proficiency (for example, through use of interpreters or translated materials).
Health equity considerations in school-based testing
Public health officials and school administrators should consider placing a higher priority for access to testing in schools that serve populations experiencing a disproportionate burden of COVID-19 cases or severe disease. These might include:
- Schools in communities that have experienced disproportionately high rates of COVID-19 cases relative to population size, which may include communities with moderate or large proportions of racial and ethnic groups, such as American Indian/Alaska Native, Black, and Hispanic persons.
- Schools in geographic areas with limited access to testing due to distance or lack of availability of testing25.
Ethical considerations for school-based testing
Testing should not be conducted without informed consent from the individual being tested (if an adult) or the individual’s parent or guardian (if a minor). Informed consent requires disclosure, understanding, and free choice and is necessary for teachers and staff (who are employees of a school) and students’ families to act independently and make choices according to their values, goals, and preferences. Differences in position and authority (i.e., workplace hierarchies), as well as employment and educational status, can affect an individual’s ability to make free decisions. CDC provides guidance and information related to consent for COVID-19 testing among employees. These considerations also apply and can be adapted to school-based testing.
Schools should make a communication plan to notify local health officials, staff, and families immediately of any case of COVID-19 while maintaining confidentiality in accordance with the Americans with Disabilities Act (ADA) external iconand Family Educational Rights and Privacy Act (FERPA)external icon, the Protection of Pupil Rights Amendment (PPRA)external icon, and other applicable laws and regulations. Collaboration with local counsel, education, or public health is recommended to ensure appropriate consent is obtained and maintained and results are retained with appropriate privacy and confidentiality.
Considerations before starting any testing strategy
Before implementing testing in their schools, K–12 school leaders should coordinate with public health officials to ensure there is support for this approach from students, parents, teachers, and staff and to develop a testing plan that has key elements in place, including:
- Dedicated infrastructure and resources to support school-based testing.
- Use of tests that are authorized by FDA for the specific intended use (i.e., screening, pooling), and a mechanism in place for prescriptions/test orders by a licensed healthcare provider.
- CLIA certificate of waiver requirements to perform school-based testing with Emergency Use Agreement-authorized tests.
- A mechanism to report all testing results (both positive and negative) as required by the state or local health department.
- Ways to obtain parental consent for minor students and assent/consent for the students themselves.
- Physical space to conduct testing safely and privately.
- Ability to maintain confidentiality of results and protect student and staff privacy.
- Plans for ensuring access to confirmatory testing when needed through the state or local health department for symptomatic persons who receive a negative test result and asymptomatic persons who receive a positive test result.
If these elements are not in place, schools may consider a referral-based testing strategy in collaboration with public health officials.
Schools should work with local public health officials to decide whether and how to use testing. K–12 schools operated by the federal government (for example, for Department of Defense Education Activity [DoDEA], which operates K–12 schools for DoD Dependents) should collaborate with federal health officials. In addition to state and local laws, school administrators should follow guidance from the Equal Employment Opportunity Commissionexternal icon, and applicable federal laws when offering testing to faculty, staff, and students who are employed by the K–12 school.
Feasibility considerations and challenges of school-based testing
These challenges must be considered carefully and addressed as part of plans for school-based testing developed in collaboration with public health officials.
- In some schools, school-based healthcare professionals (for example, school nurses) can perform COVID-19 viral testing if the school or test site receives a Clinical Laboratory Improvement Amendments (CLIA) certificate of waiverexternal icon. Some school-based healthcare professionals might also be able to perform specimen collection to send to a lab for testing, if trained in specimen collection, without a CLIA certificate. It is important that school-based health care professionals have access to, and training on the proper use of personal protective equipment (PPE). Facilities should be aware of the FDA EUA external iconfor antigen tests external iconand the Center for Medicare & Medicaid (CMS’s) enforcement discretion pdf iconexternal iconregarding the CLIA external iconcertificate of waiver when using tests in asymptomatic individuals.
- Not every school system will have the staff, resources, or training (including the CLIA certificate of waiver) to conduct testing. Public health officials should work with schools to help link students and their families, teachers, and staff to other opportunities for testing in their community.
- School-based testing might require a high degree of coordination and information exchange among health departments, schools, and families.
- There might also be legal and regulatory factors to consider with onsite school-based testing regarding who will prescribe the tests, who will administer the tests, how tests will be paid for, and how results will be reported. Such factors include local or state laws defining the services school nurses and other school-based health professionals are permitted to provide, as well as applicable privacy laws.
- The benefits of school-based testing need to be weighed against the costs, inconvenience, and feasibility of such programs to both schools and families.
- Antigen tests usually provide results diagnosing an active SARS-CoV-2 infection faster than NAATs. However, antigen tests have a higher chance of missing an active infection even in symptomatic people, and confirmatory molecular testing might be recommended.
Vaccination for teachers and staff, and in communities as soon as supply allows
Vaccination Resources for Teachers and Staff

Vaccines are an important tool to help stop the COVID-19 pandemic. Teachers and staff hold jobs critical to the continued functioning of society and are at potential occupational risk of exposure to SARS-CoV-2. Vaccinating teachers and staff is one layer of prevention and protection for teachers and staff. Strategies that minimize barriers to access vaccination for teachers and other frontline essential workers, such as vaccine clinics at or close to the place of work, are optimal. To address this important public health priority, the Health and Human Services Secretary issued a Secretarial Directivepdf iconexternal icon on March 2, 2021, that directs all COVID-19 vaccination providers administering vaccine purchased by the US government to make vaccines available to those who work in K–12 schools. This means that in addition to existing state and local COVID-19 vaccination sites, teachers and staff in schools across the nation can sign up for an appointment at more than 9,000 pharmacy locations participating in the Federal Retail Pharmacy Program for COVID-19 Vaccination.
New CDC resources are available to provide information about this directive:
- The COVID-19 Vaccines for Teachers, School Staff, and Childcare Workers web page provides school and childcare staff with the latest information about where and how to book an appointment.
- The COVID-19 Vaccine Toolkit for School Settings and Childcare Programs provides schools and childcare programs with ready-made materials they can use to communicate with staff about COVID-19 vaccination.
School officials and health departments can work together to also support messaging and outreach about vaccination for members of school communities. School communication platforms can facilitate outreach to encourage vaccination of household members of school-age children as they become eligible. This should include outreach in a language that limited English proficient family members of students can understand and in alternate formats as needed to facilitate effective communication for individuals with disabilities.
Implementation of layered prevention strategies will need to continue until we better understand potential transmission among people who received a COVID-19 vaccine and there is more vaccination coverage in the community. In addition, vaccines are not yet approved for use in children under 16 years old. For these reasons, even after teachers and staff are vaccinated, schools need to continue prevention measures for the foreseeable future, including requiring masks in schools and physical distancing.
Definitions
- School staff in this document refers to any school employees, contractors, or independent consultants interacting with students or teachers during the course of the school day, including, for example, school administration, bus drivers, school nutrition professionals, school nurses, speech/occupational therapists, custodians, and other school employees.
- https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/transmission_k_12_schools.html
- American Academy of Pediatrics. COVID-19 Guidance for Safe Schools. January 5, 2021. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/external icon
- For an example classification scheme for risk of transmission in sports, see https://ncaaorg.s3.amazonaws.com/ssi/COVID/SSI_ResocializationDevelopingStandardsSecondEdition.pdfpdf iconexternal icon
- Doyle T et al. COVID-19 in Primary and Secondary School Settings During the First Semester of School Reopening – Florida, August-December, 2020. MMWR 2021; March 19, 2021.
- Hershow RB et al. Low SARS-CoV-2 Transmission in Elementary Schools – Salt Lake County, Utah, December 3, December 3, 2020-January 31, 2021. MMWR 2021; March 19, 2021.
- Volpp KG et al. Minimal SARS-CoV-2 Transmission Following Implementation of a Comprehensive School Mitigation Strategy – New Jersey, August 20-November 27, 2020. MMWR 2021; March 19, 2021.